Health Care Access in Appalachia and the Coronavirus Pandemic

As of Tuesday night, every state in the U.S. has at least one positive case of the novel coronavirus. In Appalachia, health care providers are growing increasingly concerned about the capacity of their rural health care systems and the overall health and social determinants that might leave the region’s citizens at higher risk for a more serious case of the virus.
“We do not want to overwhelm our health care. We don’t want everyone coming at once and overwhelming the hospital,” Dr. Kathryn Moffett, a pediatric infectious disease specialist at West Virginia University Medicine Children’s, said in by WVU Health Sciences. “We want to spread out infection and not overwhelm our hospitals to be able to treat everyone and keep everyone safe.”
The virus most seriously affects people over 65, people who are immunocompromised, and those who have serious chronic medical conditions, including respiratory conditions such as asthma and COPD, according to the . As medical centers across the region focus on increasing their capacity to test for the virus, the statistics below provide a better understanding of the access and general health of the region.
Access to Care
Uninsured
According to the latest numbers available from the , more than 28.5 million Americans were uninsured in 2018, or 8.5%. In the 13 states that lie either in part or fully in Appalachia, the rates of uninsured vary drastically.
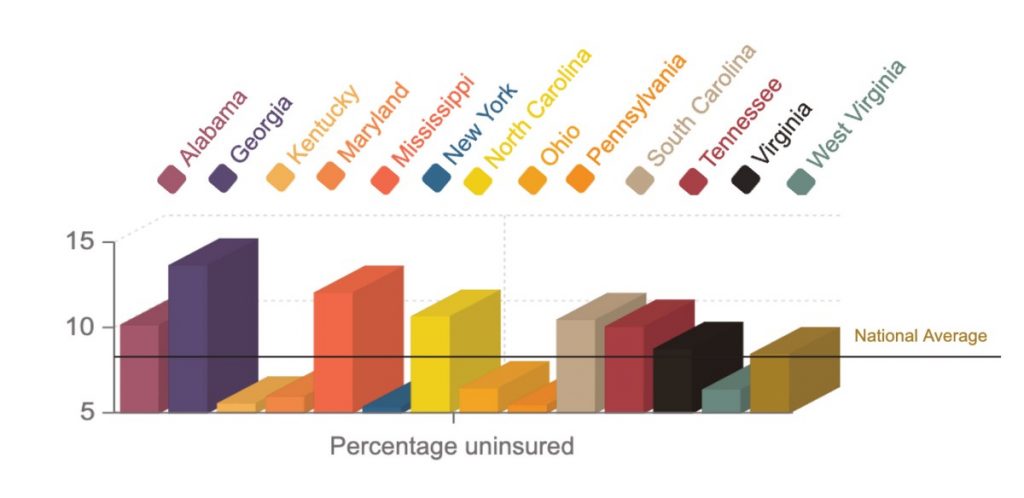
Those Appalachian states with the highest rates of uninsured have not expanded Medicaid as allowed under the 2010 Affordable Care Act, which provided states with extra financial support to provide a larger group of lower-income Americans access to the government health insurance.
Kentucky, New York, and Pennsylvania all have the lowest rates of uninsured residents, ranging from 5.4 to 5.6%. Kentucky and New York adopted the Medicaid expansion policies in 2014, with Pennsylvania following in 2015.
The highest rates of uninsured residents are in the Appalachian states of Georgia, at 13.7% and Mississippi, at 12.1%. Alabama, North Carolina, South Carolina, and Tennessee all have rates higher than 10%, as well. haven’t expanded Medicaid.
Travel Time and Beds
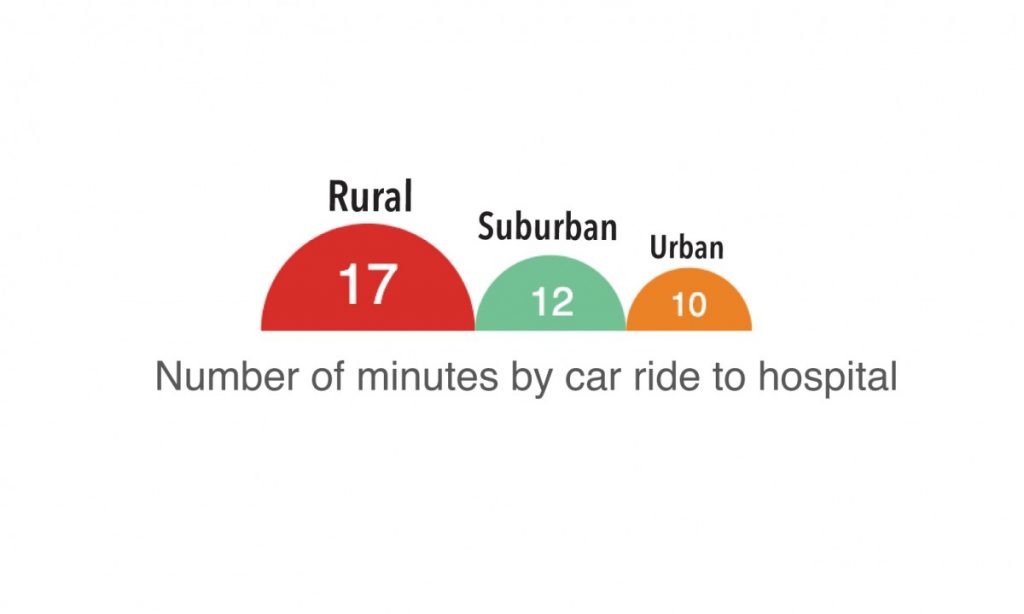
As hospitals close in rural communities across the region, the amount of time it takes to reach a hospital has increased and the number of beds available once you get to those hospitals has decreased.
The in 2018 measured the distance on average for people living in rural, suburban, and urban areas in the U.S. to the nearest hospital and used traffic patterns in those places to convert the distance to minutes. The study found for Americans living in rural communities – the reports 42% of people in the region live in rural areas – it takes on average 17 minutes to reach the nearest hospital.
Nationally, the , a nonprofit organization that studies national health issues, reports that 2.4 hospital beds are available for every 1,000 Americans. In Appalachia, access fluctuates by state.
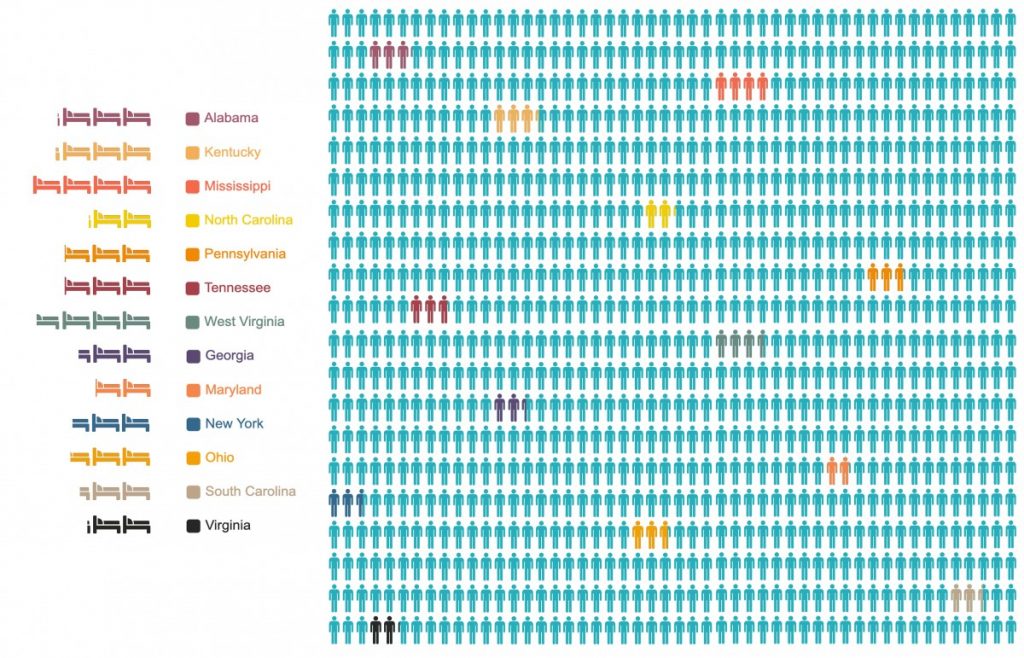
Mississippi and West Virginia, states that are known for having traditionally low health outcomes, have the highest number of beds available per 1,000 residents, at 4 and 3.8 respectively. On the opposite end, Maryland, North Carolina, and Virginia have the fewest beds per 1,000 people, with Maryland at 1.9 and North Carolina and Virginia both at 2.1 beds.
General Health
Poverty
National guidelines set the in 2020 at $26,200 for a family of four. The latest numbers available from the say that in 2018, 11.8% of Americans lived at or below the federal poverty level.
Income has a direct correlation to overall health and ability to access health care, and in Appalachia, rates of poverty are higher in many states than the national average.
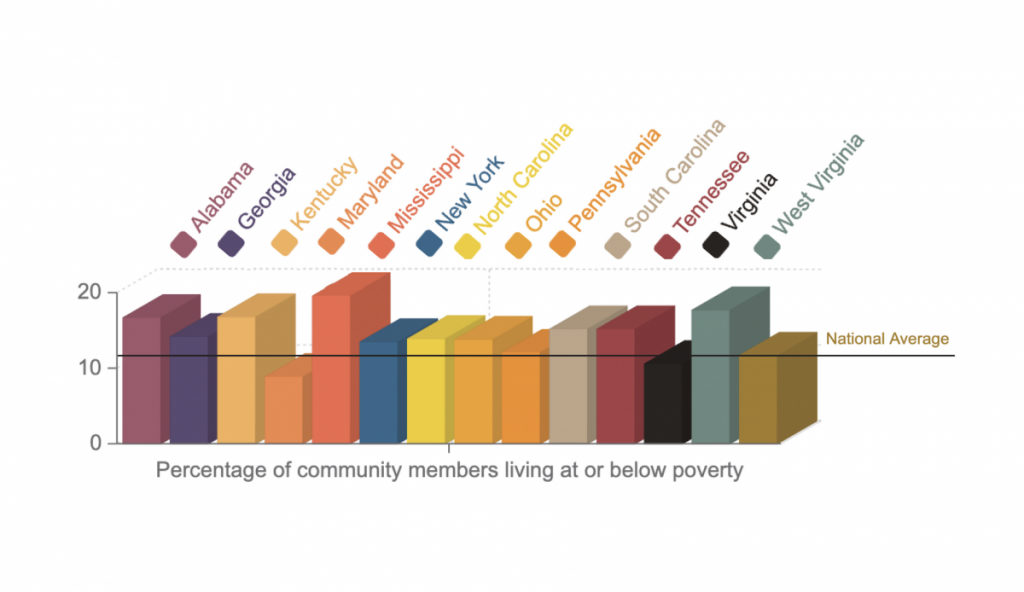
Mississippi struggles with the highest rate of poverty in the region and, in turn, nationally at 19.7%, followed closely by West Virginia, at 17.8%, Kentucky, at 16.9%, and Alabama, at 16.8. Maryland is the only state with a single-digit poverty rate in the region, at 9%.
Age
Individuals over 65 are designated as being at higher risk to experience more serious symptoms of the virus than younger individuals, some of whom may be carriers without experiencing symptoms themselves, . Nationally, 16% of the population is over age 65, according to data from the .
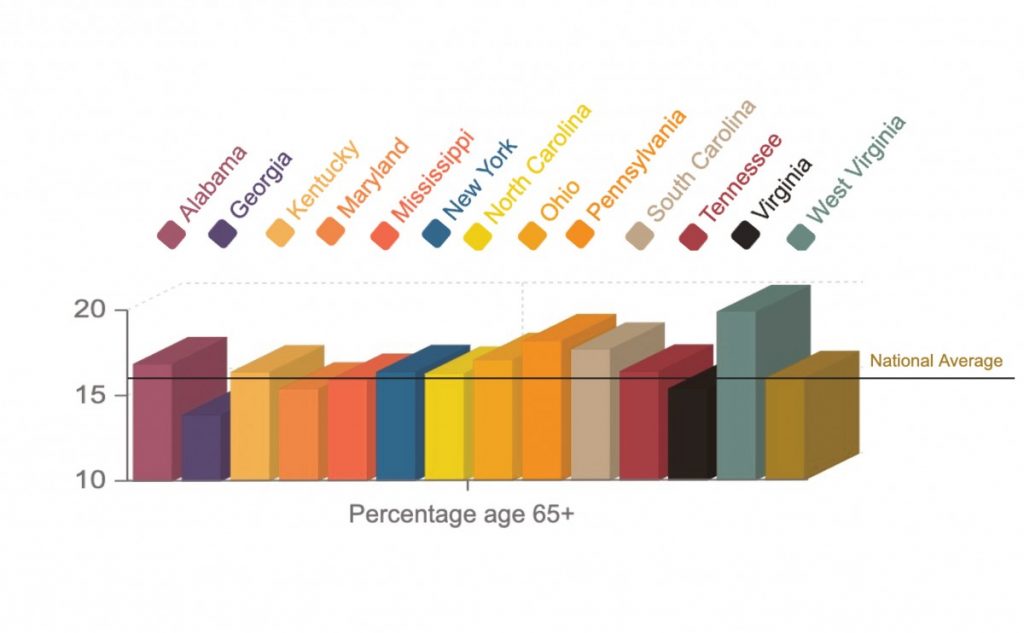
In most Appalachian states, the percentage of the population over the age of 65 mimics that of the national average. Three states have more than 1% of the population higher. West Virginia has the largest percentage of older residents at 19.9%, according to data from the , among the top three oldest states in the country. Pennsylvania, at 18.2%, and South Carolina, at 17.7%, are the closest behind.
Georgia, Maryland, and Virginia have the lowest percentage of residents over age 65.
Diabetes
Diabetes is not listed by the CDC as one of the chronic illnesses that increases the risk of complications of the coronavirus, but the health condition itself can lead to more serious health problems and lessen the overall health of an individual. Nationally, more than 9% of Americans has diabetes, .
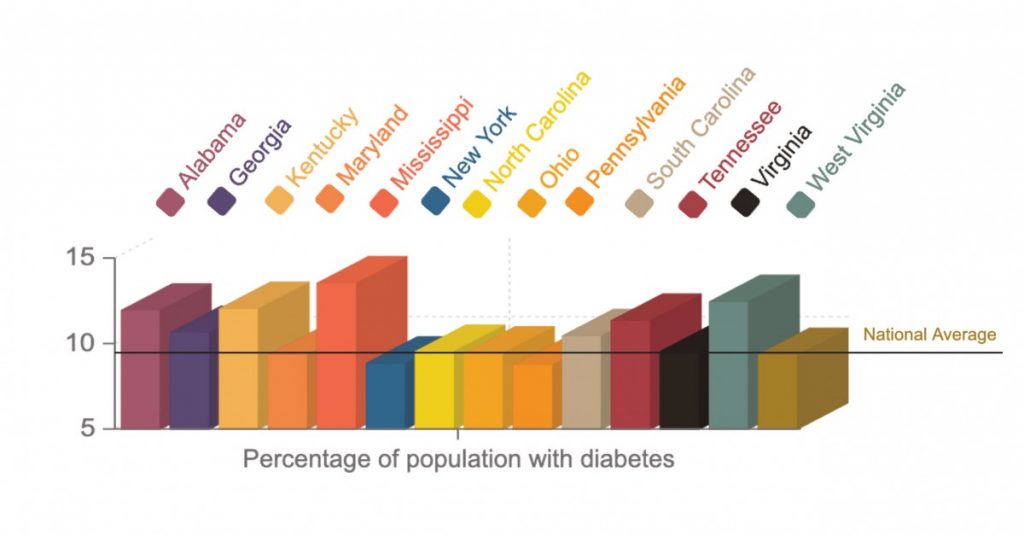
In Appalachia, Mississippi and West Virginia have the highest rates of their population living with diabetes, at 13.6 and 12.5 respectively. Alabama, Georgia, Kentucky, South Carolina, and Tennessee all have rates over 10%, while Pennsylvania and New York both have rates just under 9%, at 8.8 and 8.9.
Smoking
CDC guidelines warn individuals with respiratory issues to take special precautions to protect themselves from the novel coronavirus. Smoking can increase a person’s risk of experiencing more severe symptoms of the virus and can also . Nationally, 13.7% of Americans are smokers, .
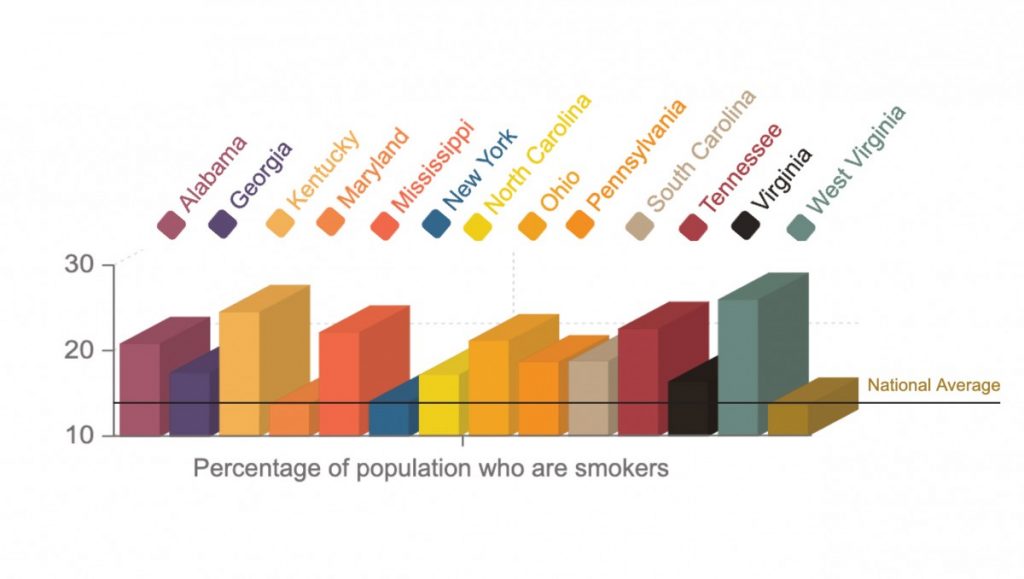
In most Appalachian states, rates of smoking are well above the national average. In fact, no state in the region has a rate lower than the nation. The highest rates come in West Virginia, at 26%, Kentucky at 24.6%, Tennessee at 22.6% and Mississippi at 22.2%.
This article was originally published by . It has been published here with permission.





